- Your cart is empty
- Continue Shopping
Zopiclone: A Comprehensive Guide to Its Mechanism, Uses, and Research
Sleep is a vital biological function, yet not everybody is privileged to get enough sleep to get their system running seamlessly. Studies and researches have concluded that 10–30% of the adult population suffer from chronic sleep disorders along with other sleep related issues have been associated with cognitive impairment, poor metabolism, and mood disorders.
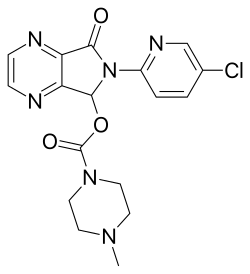
Image source: https://en.wikipedia.org/wiki/Zopiclone
Zopiclone has been studied thoroughly as a short-term treatment for insomnia or chronic loss of sleep. This article guides you through how this medicine works for insomnia, and how to take it. As you read along, you will learn about the side effects of Zopiclone, and the preventive measures you must follow while taking this medicine. We will also going to explore the drug interaction aspect of the insomnia treatment. Which medicine goes well with the sleep-inducing medicines and which one to avoid in order to prevent unpleasant interactions and associated ill effects; we are going to see all of this. And, we will also learn recent research findings about the medicine. Keep reading!
What Zopiclone Is and How It Works
It belongs to the class of drugs called cyclopyrrolones, commonly known as “Z-drugs.” Zopiclone is chemically different from benzodiazepines, but it acts on the GABA-A receptor complex. It causes sedation and hypnotic effects by boosting the inhibitory effects of GABA.
This medicine has a short half-life which is about 5 hours, and it allows inducing sleep without extended residual sedation in most patients. Furthermore, the drug increases sleep duration, and decreases sleep latency (time taken to fall asleep). However, this medicine does not change the natural sleep cycle as radically as conventional benzodiazepines, as per the polysomnography studies.
Clinical Use and Indications
Zopiclone is majorly prescribed for short-term treatment of insomnia. It is basically given to individuals who have difficulty falling asleep or staying asleep. This medicine is given when non-pharmacological treatments such as Cognitive Behavioral Therapy for Insomnia and sleep hygiene measures are inadequate or unfeasible for offering immediate relief.
Medical authorities have issued guidelines for Zopiclone usage for insomnia. As per those guidelines, this medicine should be used for a time span of 2 to 4 weeks. This time span is curated on the basis of the risk of dependence, tolerability, and rebound insomnia with long-term usage of the medicine.
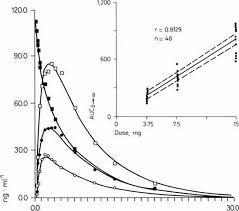
Dosage and Pharmacokinetics
This Zopiclone guide will help you understand basic dosage measurements given to adults. However, this information does not replace medical advice. One must consult a doctor to get accurate dosing pattern as per their medical history and current medical status.
- The standard dosage is 7.5mg which is taken at least 30 minutes prior going to bed.
- Elderly patients must start their treatment with the lowest dosage which is of 3.75 mg due to low metabolism and higher risk of developing side effects.
The medicine gets absorbed in the blood with peak plasma concentration occurring in 1 to hours. it gets metabolized in the liver through CYP3A4, and excreted through kidneys.
Efficacy: What Research Shows
Several clinical trials and meta-analyzes have studies efficiency of Zopiclone, and concluded that this medicine can:
- Diminish sleep latency by approximately 30–40%
- Increase total sleep time by up to one hour
- Prevent intermittent sleep
However, these advances are generally modest, and some studies note that subjective measures of sleep quality often show greater alleged benefit than objective polysomnography findings.
A 2020 systematic review in Sleep Medicine Reviews evaluated Z-drugs, including Zopiclone, and stated that while these drugs are effective for short-term insomnia, their long-term benefits stay unverified, and non-drug interventions remain the mainstay for chronic insomnia.
Safety Profile and Side Effects
Zopiclone is generally well-tolerated when used correctly, but it carries impending side effects, including:
- Bitter or metallic taste in the mouth
- Dry mouth
- Daytime drowsiness or mild cognitive impairment
- Dizziness or coordination difficulties
Rarely, sleep-related behaviors such as sleepwalking, sleep-driving, or performing complex tasks while not fully awake have been reported. Older adults are particularly at risk of falls, fractures, and cognitive impairment, which is reflected in guidance from the American Geriatrics Society recommending caution in this population.
Dependence, Tolerance, and Withdrawal
Although Zopiclone was developed to have lower dependence potential than benzodiazepines, prolonged use can lead to tolerance and physical dependence. Withdrawal symptoms may include rebound insomnia, anxiety, irritability, and tremor. Epidemiological studies suggest that 7–10% of users continuing treatment beyond 6 weeks may develop signs of dependence. Gradual tapering under medical supervision is recommended to minimize withdrawal effects.
Drug Interactions and Precautions
Zopiclone should be used cautiously or avoided in combination with:
- Alcohol, which can increase sedation and respiratory depression risk
- Opioids or antihistamines, which may amplify central nervous system depression
- Other CNS depressants, which may increase cognitive and motor impairment
Individuals with severe hepatic impairment, respiratory disease, or untreated sleep apnea should generally avoid Zopiclone due to heightened risk of adverse effects.
Pregnancy and Lactation Considerations
Limited data exist regarding Zopiclone use during pregnancy. Potential risks include neonatal respiratory depression and maternal sedation. Consequently, use during pregnancy is generally avoided unless benefits outweigh risks. Similarly, Zopiclone can pass into breast milk, and caution is advised during lactation.
Alternatives and Modern Perspectives
Recent research has introduced alternative pharmacological options, such as dual orexin receptor antagonists (e.g., suvorexant), which target the wakefulness system rather than the GABAergic system. Non-pharmacological strategies, including CBT-I, remain the first-line intervention due to efficacy and safety advantages. Studies indicate that combining behavioral therapy with short-term pharmacological treatment may optimize outcomes.
Current Research Trends
Recent literature has focused on:
Cognitive and psychomotor effects: Studies suggest subtle impairments may persist even after acute use.
Personalized medicine: Genetic variability in liver enzymes (e.g., CYP3A4) affects drug metabolism, indicating a potential role for individualized dosing.
Comparative efficacy: Research continues to evaluate Z-drugs against newer hypnotics and non-drug interventions for chronic insomnia management.
Overall, the consensus is that Zopiclone is useful as a temporary intervention but not as a long-term solution.
Final Thoughts
Zopiclone is a well-studied non-benzodiazepine hypnotic used for short-term insomnia treatment. Its mechanism of enhancing GABAergic inhibition provides sedation and improved sleep continuity. While effective for immediate relief, its use is limited by potential dependence, withdrawal, next-day sedation, and cognitive effects, particularly in older adults. Current research emphasizes careful, short-term application, combined with non-drug strategies, for sustainable sleep improvement.
In the context of modern sleep medicine, Zopiclone serves as a temporary aid, while behavioral interventions remain the cornerstone of long-term insomnia management.